Many people have questions about their medicines that their doctor doesn’t have time to answer. Medication Insider has clear, practical answers to your medication questions to help you take your medicines and supplements SAFELY.
Helping You Take Your Medicine Safely
The Top 10 Pitfalls of Mail Order Pharmacy and How to Beat Them
Download Article
Previous
Next
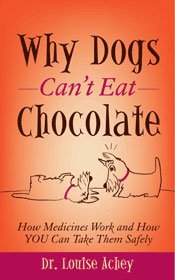
Why Dogs Can't Eat Chocolate: How Medicines Work and How YOU Can Take Them Safely
THE MEDICATION INSIDER BLOG

May always reminds me of my mother, but not just because of Mother’s Day.

I can’t stand fried chicken. I never go to KFC, and at potlucks I’ll

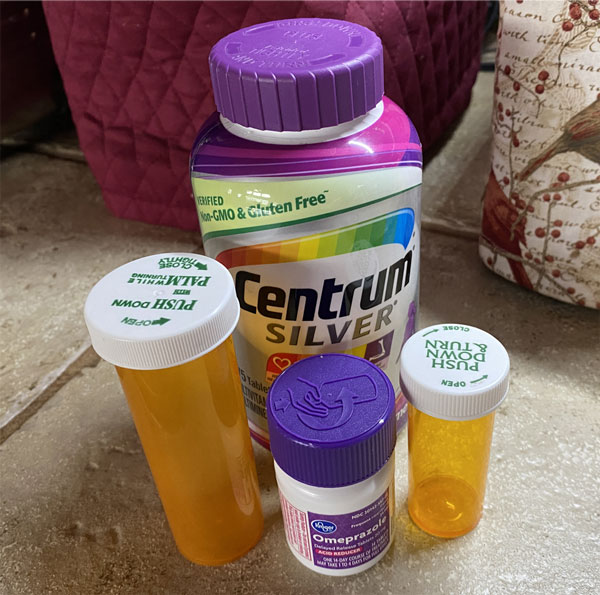
Flu season is here. It’s time to check my medicine cabinet. Do I have
This summer, many families are planning and attending events that have been postponed due

Q: I take Tylenol® for fever or headaches because it doesn’t upset my stomach
Last Saturday morning Kathy and her best friend Ann were on a video conference